Abstract
Introduction
Population-based studies have demonstrated improved outcomes for patients with multiple myeloma (MM) treated at high volume facilities (Go RS et al. JCO 2017;35(6):598-604). Our objective was to examine the effect of treatment at an NCI Comprehensive Cancer Center (NCICCC) and specifically by a myeloma specialist on overall survival (OS). We also sought to evaluate the impact of patient sharing between NCICCC myeloma specialists and community oncologists on outcomes for patients.
Methods
Using the University of North Carolina Lineberger Cancer Information and Population Health Resource (CIPHR), a database that links Medicare, Medicaid and private insurance claims to the North Carolina Cancer Registry, we identified a cohort of patients diagnosed with MM from 2006 to 2012.
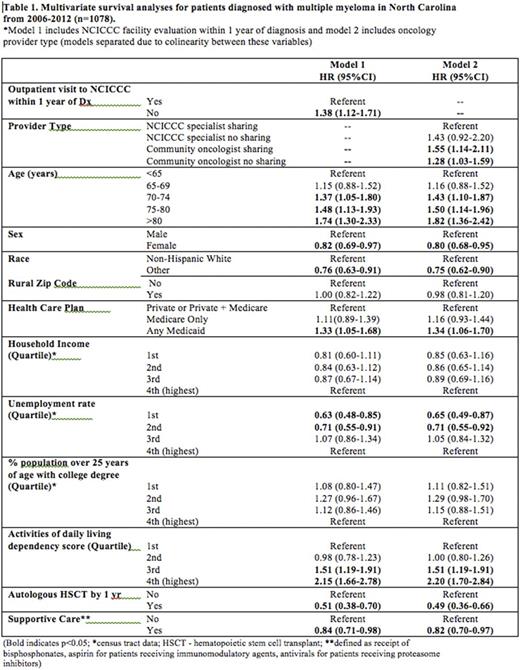
Two multivariable Cox models were used to explore OS differences. The first examined the impact on OS of at least 1 visit to an NCICCC within 1 year of diagnosis. The second examined the impact on OS of 4 mutually exclusive patient categories based on the type of primary oncologist: 1. an NCICCC myeloma specialist who does not have a history of sharing patients with community oncologists; 2. an NCICCC myeloma specialist who shares patients with community oncologists; 3. a community oncologist who does not have a history of sharing patients with an NCICCC myeloma specialist; 4. a community oncologist who shares patients with an NCICCC myeloma specialist. Patients' most visited oncologist was deemed the primary oncologist. A list of myeloma specialists was defined through consensus among representatives from the 3 NCICCCs in North Carolina.
Covariates for both models included age, sex, race, insurance type, urban versus rural home address, socioeconomic indicators based on census tract information for residential zipcode (median household income, unemployement, education), receipt of autologous bone marrow transplantation and receipt of supportive care (bisphosphonates, aspirin for patients receiving immunomodulatory agents, antivirals for patients receiving proteasome inhibitors).
Results
One thousand seventy eight patients with newly diagnosed MM were identified. Mean age at diagnosis was 68 years (range 28-98 years), 48% of patients were male, 65% were non-Hispanic white, 43% had private insurance alone or in combination with Medicare. Approximately half (49%) were seen at an NCICCC clinic within 1 year of diagnosis. Fifty six per cent of patients were primarily treated by a community oncologist who did not have a history of sharing patients with NCICCC myeloma specialists, 31% by an NCICCC myeloma specialist who shared with community oncologists, 9% by community oncologists who shared with NCICCC myeloma specialists and 4% by NCICCC myeloma specialists who did not share with community oncologists.
In the first multivariate analysis examining the impact of NCICCC evaluation, the absence of a visit to an NCICCC was associated with worse OS (HR 1.38, CI 1.12-1.71, p<0.01). In the second multivariate analysis examining the impact of provider type, we found that compared to patients primarily treated by NCICCC myeloma specialists, patients primarily treated by community oncologists who either share or do not share patients with NCICCC specialists had worse OS (HR 1.55, CI 1.14-2.11, p<0.01 and HR 1.28, CI 1.03-1.59, p<0.05 respectively).
Covariates significantly associated with worse OS in both models included increasing age (eg. age >80 years HR 1.74, CI 1.30-2.33, p<0.001) and Medicaid insurance (HR 1.33, CI 1.05-1.68, p<0.05). Receipt of autologous bone marrow transplantation (n=179, 17%) and supportive care were associated with improved OS (HR 0.51, CI 0.38-0.70, p<0.001 and HR 0.84, CI 0.71-0.98, p<0.05 respectively) (Table 1).
Conclusions
Using CIPHR, a statewide linked tumor registry and claims database, we found that patients seen at an NCICCC outpatient facility within 1 year of diagnosis and those treated primarily by NCICCC-affiliated myeloma specialists had superior OS compared to those who did not. This may reflect a higher volume of MM cases, increased availability of supportive services, or greater access to clinical trials and hematopoietic stem cell transplantation at NCICCCs. Further examination of the impact of additional socioeconomic variables, individual provider MM patient volumes and local treatment patterns may yield insights that can inform strategies to improve MM outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal